Munira Abdi and her husband suspected their son, Salam, may have developmental issues when he stopped talking at 18 months old and started crying frequently. At the age of 4, they confirmed Salam had Autism Spectrum Disorder (ASD).
As Salam grew, his parent’s biggest challenges were to keep him safe and to get any communication or response from him. He didn’t have an understanding of danger and would dart into traffic if not watched carefully.
After a frustrating 6-month wait to access services, Salam received speech therapy and Applied Behavior Analysis (ABA) through Seattle Children’s Autism Center and an Individual Education Plan (IEP) at school.
Knowing they needed to develop Salam’s safety awareness and communications skills, Munira recalled, “once we found out our son was autistic, we wanted to do everything for him. We wanted to get him therapy.”
However adding financial stress to a challenging time, the family’s insurance company, Aetna – Sound Health & Wellness Trust, denied Salam’s ABA therapy. Having therapy denied after such a long wait added insult to injury.
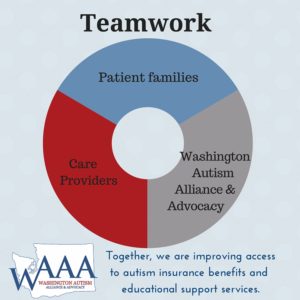
Seeking help anywhere she could, Munira reached out for assistance. Trish Thrush, WAAA insurance advocate, teamed with Michelle Sauncy from Connections Behavior Planning & Intervention to help Munira file an insurance appeal after the initial claim was denied. Michelle was invaluable to the appeal process; filing claims, speaking to the insurance company and providing documentation of medical necessity. Trish commends Michelle’s contributions, “Michelle was extremely supportive of the family and the process. Michelle’s dedication to her clients is heartwarming and inspiring.”
While drafting an appeal to Aetna on the basis that blanket exclusions for ABA violate Mental Health Parity Laws, WAAA’s Family Support team advised Munira to get an individual insurance policy with Molina through the Washington Health Benefit Exchange to cover out-of-pocket expenses. An additional denial from Molina added to the frustration, as all State plans must cover medically necessary therapy. Michelle refused to accept the denial and within a week was successful in getting Molina to correct the mistake.
“My son isn’t the only child,” attests Munira. “He is not the first one and won’t be the last.” Pointing out the fundamental right to meeting a child’s medical needs, Munira hopes that some day other families won’t have to go through similar struggles. She encourages parents to have specialists, pediatricians, and insurance companies work together to assemble the medical documentation and language necessary to ensure coverage.
Munira’s efforts have paved the way for more children with autism to get ABA covered by insurance. Her appeal resulted in removal of the ABA exclusion in plans administered by Sound Health & Wellness Trust for multiple employers, including Zenith Administrators, Safeway, Albertsons, Fred Meyer, QFC, Bartell Drugs, and Rite Aid.
Munira appreciates the support from WAAA and her ABA providers to navigate rough insurance waters, “if it wasn’t for WAAA, we wouldn’t have been so fortunate. Our son is in therapy right now and is doing very well.”
Sauncy noted that WAAA is a great resource for both parents and providers, recognizing that WAAA not only helps with paperwork, but also provides family support along the way.
As a provider, Sauncy hopes to team with WAAA on more appeals in the future to help families get the services their kids need. She advises parents, “The tide is turning. Find a provider who will help you navigate tough situations. Find support groups and forums to share and learn.”
Together, we are building a community of supporters to help families meet their children’s educational and medical needs.