An interview with Linda Meyer, EdD, MPA,BCBA-D, and Jeff Jacobs, MA, BCBA
Published June 12, 2013
This article appears under Physical Fitness, General Health & Wellbeing › Sports & Exercise;
by David Celiberti, Executive Director of the Association for Science in Autism Treatment
I recently had the opportunity to interview two very talented behavior analysts, Linda Meyer and Jeff Jacobs, who answered a wide array of questions about fitness programming for individuals with autism. Their unique experiences as behavior ana-lysts and fitness consultants (Linda is a certified personal fitness trainer and marathon runner; Jeff is a black belt in martial arts and a runner) have clearly shaped their perspectives on how to pro-mote fitness behaviors in individuals with autism.
Jeff, much of the existing, published research has focused on the use of exercise to address challenging behaviors in persons with autism. Can you provide a synopsis of this literature, along with its recurring themes, and perhaps share your thoughts on future directions within this area?
Yes, numerous studies have demonstrated decreased stereotypy in children and adults with autism following physical activity. Stereotypic behavior decreased significantly following jogging in three men and three women with autism of ages ranging from 22.8 to 41.3 years (Elliot, Dobbin, Rose, & Soper, 1994). Aerobic exercise was found to reduce the stereotypical behavior patterns and self-stimulatory behavior of children with ASDs (Elliot, Dobbin, Rose, & Soper, 1994). Ten minutes of roller skating prior to a structured play session decreased self-stimulation in an eight-year-old boy with developmental disabilities (Powers, Thidabeau, & Rose, 1992). Rosenthal-Malek and Mitchell (1997) observed that self-stimulatory behaviors decreased, correct responding increased, and the number of tasks completed increased following physical fitness activities (versus academic activities) in adolescents with autism. Celiberti, Bobo, Kelly, Harris, and Handleman (1997) observed that suppression of stereotypy following jogging remained below baseline levels for up to 40 minutes. After an 8–10-minute jogging session outside a school building, Watters and Watters (1980) observed lower levels of self-stimulation for five males with autism, aged 9 to 11 years. Yilmaz,Yanardag, Birkan, and Bumin (2004) observed reduction in topographies of stereotypy in a nine-year-old immediately following swim sessions.
The speed, frequency, and intensity of the aerobic activity appear to be significant intervening variables (Dunn, 1984; Kern, Koegel, & Dunlap, 1984; Levinson & Reid, 1993). Walking had limited, if any, impact on reducing stereotypy. Increased speed decreased stereotypy (Allison, Basile, & MacDonald, 1991; Levinson & Reid, 1993; Elliot et al., 1994). Prupas and Reid (2001) demonstrated a slight reduction in stereotypy across four children, ages five to nine years, when tenminute jogging sessions were increased from one to three sessions per day.
In summary, there is research demonstrating the effectiveness of exercise to reduce stereotypy. Further research is required to determine how the interrelated characteristics of amount, intensity, frequency, and type of physical activity are related to the topography, duration, and magnitude of decrements in stereotypy. There are no clear guidelines from research to guide the development of an exercise routine to effectively and consistently reduce stereotypy for an extended period of time. A 2010 review by Lang, Ashbaugh, Regester, Ence, and Smith suggests that physical stimulation during exercise might replace or reduce motivation for the individual to engage in motor stereotypy. Exercise may also act like a prolonged overcorrection procedure or a differential reinforcement of incompatible behavior (DRI) or differential reinforcement of other behavior (DRO) that research has shown to be effective for decreasing stereotypy (Ahearn, Clark, MacDonald, & Chung, 2011).
Linda, clearly there are other advantages beyond the mere suppression of stereotypy. Can you provide our readers with some of the positive outcomes associated with targeting fitness in children and adults with autism?
Targeting fitness is a great idea for many reasons. We know that regular exercise can promote health and fitness as well as improve appearance. Achieving an appropriate fitness level can help individuals with autism spectrum disorders participate more fully with their families in leisure time activities and everyday household chores, as well as within educational, vocational and community environments. More specifically, participation in fitness programs can: 1) improve social and communication skills (Pan, 2010); 2) improve heart and lung functioning; 3) improve balance and flexibility (Yilmaz, Yanardag, Birkan, & Bumin, 2004); 4) strengthen muscle; and 5) increase lean body mass.
Lochbaum and Crews (2003) taught five individuals with autism, ages 16 to 21; three participants learned to ride a stationary bike and two were taught to lift weights on a Nautilus ® exercise machine. All participants improved in aerobic and strength fitness. Using a treadmill, Pitetti, Rendoff, Grover, and Beets (2007) reduced the body mass index (BMI) of ten adolescents with severe autism and increased their exercise capacity (i.e., participants walked faster and longer with increased incline). BMI is a number calculated from a person’s weight and height. It provides a reliable indicator of body fat for most people and is used to screen for weight categories that may lead to health problems.
Engaging in specific exercises and related sports activities repeatedly promotes skill development in those specific exercises or sports activities. For example, Fragala-Pinkham, Haley, and O’Neil (2008) observed a significant reduction in the amount of time for six male adolescents on the autism spectrum to complete a halfmile run/walk.
In July of 2011, the Centers for Disease Control and Prevention /American College of Sports Medicine (ACSM) released a policy statement summarizing recommended exercise components and the health benefits supported by scientific studies. The overall message is for individuals to get involved in a comprehensive program of exercise, reduce time spent in sedentary activities and spend more time moving.
So Jeff, what would you recommend as the first step, when selecting a fitness program for an individual with autism?
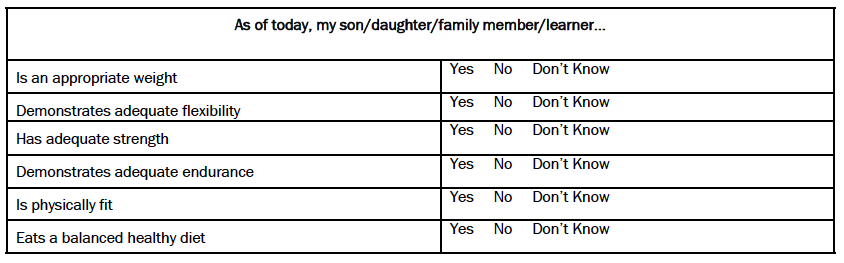
A comprehensive exercise program includes flexibility, cardi-orespiratory, and strength training exercises; however, it is important to select a program based on your desired outcome. Decide if you want to increase flexibility, heart endurance, respiration, muscle strength or any combination. Begin with the outcome in mind. What are the benefits you are hoping to achieve through participation in an exercise program? We have developed a checklist (Meyer & Jacobs, 2007) to help you select the right program.
Linda, can you tell our readers more about how this checklist can be used to determine if an exercise program is a good fit for an individual with autism? Can you also mention where the checklist is available, and if it is easily accessible?
It is generally recognized that a limited number of fitness and recreation programs are available to participants with autism spectrum disorders. Consider: the cost; proximity to home/school/work; staff qualifications; cleanliness; and the program’s philosophy and ability to meet personal goals, and always keep the individual safe. Our checklist can assist participants and/or the families and professionals who support them in evaluating a potential recreation or fitness program. The checklist can remind you to collect details regarding: the age appropriateness of the activities; how skills are taught, generalized, and maintained; the ability to use motivational systems; and how programs are evaluated and progress is measured. We strongly urge you to observe the program in person, and use this checklist to guide your conversations with everyone.
Observing the program and using our checklist can help you determine if your goals can be met in a particular program that is designed and monitored by the trainer. For example, is the exercise session long enough and at correct intensity, duration and frequency level to actually promote heart and lung conditioning? If socialization is one of your participant’s goals, repeated opportunities to practice and/or learn new social skills (e.g., initiating, commenting, responding to comments from others) must be built into the program.
Are there any other suggestions or steps to consider before enrolling or participating in a fitness program?
We have a few more suggestions:
- Obtain a complete health assessment and medical history. It is important to receive medical clearance before beginning any exercise program.
- Many facilities have special membership deals if the participant is able to work out during off-peak hours (usually mid-to-late afternoon).
- Do not compromise with respect to clothing. Buying workout attire suitable for the specific workout promotes a socially acceptable, safe and healthy workout.
- If a participant with autism does enroll in a fitness program, it is critical to address all safety concerns and develop routines that will maximize the fitness benefits.
- During workouts, always arrange the environment and provide schedules to promote active engagement and independence. Schedules can be in various forms, including: written, photographic, spoken instructions, and/or a combination on an iPad or a notebook.
As Jeff mentioned, you need to assure safety and maximum fitness benefit during a fitness workout or community recreation event. Monitoring levels and types of stereotypy is important, but vocal and motor stereotypy may not necessarily be stigmatizing. If you observe all of the competitors at the start of a running race or individuals engaging in strength training routines at a gym, you will more than likely see many of them rocking and/or pacing back and forth to music from their iPods (especially during the brief rests between weight training sets in gyms) and high rates of unusual, repetitive body movements before a race. Recently I noted a new rule posted in the weight room of the gym where I work out. It stated: “No loud grunting.” To the best of my knowledge, no one with autism had been working out in that gym.
Our readers will appreciate that very comprehensive set of considerations. Linda, let’s get into the details about support systems. What information about autism would be important to share? What is needed to make a fitness program successful?
Individuals with autism may be unresponsive to instructions from their fitness trainers or requests to perform exercise routines and tasks, have limited communicative ability, and be unaware of safety issues and potentially dangerous situations. Make sure everyone is on board and understands the individual’s fitness goals. Those involved should support the individual’s needs, strengths, and competencies (e.g., can follow a written schedule), as well as his/her unique characteristics of autism.
To increase the potential for success, spend time talking with the program’s director/owner, as well as the supervisors/trainers who will be conducting the fitness sessions. You may need a team: someone who understands autism, someone who knows the principles of exercise science, and someone experienced in teaching skills. You may consult with a Board Certified Behavior Analyst (BCBA®) for guidance on teaching skills, and fitness trainers to provide advice on exercise routines, fitness goals, and safety. Consider selecting a teacher and/or support person who works out her/himself.
If you cannot afford or find a team, consider recruiting volunteers who are willing to be trained. Many graduate exercise science programs require volunteer and internship hours. High schools commonly require students to perform community service hours. Consistency and communication amongst members of the team will be essential to ensure success.
Jeff, what behavior analytic teaching procedures bear relevance to the teaching of fitness skills?
The teaching procedures most frequently reported in the literature to teach exercise behavior include providing verbal and tangible reinforcement, use of systematic prompting hierarchies with prompt fading, modeling (video and in-vivo) with verbal instructions, and physical guidance using a least-to-most prompting procedure.
It might be helpful if we described the use of a least-to-most prompting procedure to teach a strength training skill: the bicep curl (biceps are muscles located in the upper arm to help you hold heavy objects) to a 17-year-old female with autism. Katie would benefit from resistance training, as resistance or strength training promotes an increase in bone strength, which reduces the risk of musculoskeletal injuries or perhaps the severity of those injuries (Kohrt, Bloomfield, Little, Nelson, & Yingling, 2004). We will use a least-to-most prompting procedure combined with an errorless teaching procedure (Yanardag, Birkan, Yilmaz, Konukman, Agbuga, & Liberman, 2011).
Target Skill:
Biceps Curl: Katie stands with feet hip width a part, knees slightly bent, arms at her sides, palms up and holds a barbell at waist height. Keeping elbows close to her body, Kathy curls both arms up until they are in front of her shoulders. Then she lowers the barbell down to the original position.
Suggested Teaching Steps:
- Probe: holds lightest free weight barbell available (<10 lbs. or 1.5” diameter wooden dowel). Trainer holds a similar barbell, faces the client and says, “Do this,” and then begins a correct biceps curl. If the client imitates a good approximation of the trainer’s barbell movement, provide verbal praise. The client is ready to begin using the barbell. Increase the weight of the barbell until baseline is established and start training.
- If no imitation, present a tangible reinforcer and say, “Do what I am doing and you will get _____.” If acceptable imitation, present reinforcer accompanied by verbal praise and follow training objectives incorporating a motivation system.
- If no imitation, demonstrate the curl again and provide physical guidance. Stand behind the client and position your hands on the barbell with each of your hands located slightly outside of the client’s hands. Reinforce with tangible and verbal praise.
Fade the position of the physical prompt (e.g., from barbell to client’s forearms), shadow client’s hands, use moving gestural prompt, no prompts until the client performs the barbell curl independently.
Suggested Alternative:
If your client is unable to perform a standing barbell biceps curl, consider moving to a piece of equipment in the gym called the biceps curl machine.
Linda, what role can parents play in supporting the program and promoting carryover? Can you share any specific examples of how this may play itself out?
Recent research suggests that parents play an important role getting and keeping their children involved in fitness programs (Nelson, Gordon-Larsen, Adair, & Popkin, 2005). As individuals with autism may be unable to independently demonstrate an interest in, or determine a need for a type of a fitness program, parents frequently play these critical roles. Traditionally, when any family member participates in a sport or fitness program, it impacts the entire family. Parents need to be able, willing, and agree to dedicate family resources (e.g., time, money, transportation) to begin and continue a meaningful fitness program for their family member with autism. We’ve observed that when an individual with autism gets involved in regular fitness activities, more often than not, moms and dads, as well as teachers and support persons also begin to participate.
To assess the impact a running club had on families at the Eden II School in Staten Island, Randy Horowitz distributed a survey to determine how often parents participated in exercise routines with their children. Prior to the running club, 20% of parents reported that they had participated with their child in any exercise program. Seven months after the running club began, the same families were surveyed again, and 23 out of the 35 (66%) respondents indicated that they had participated in exercise routines with their children.
Parents are now running with their children in the park or at the track of the local YMCA, which is also where the participants run weekly with the school-based running club. One mom and dad reported that they had never run in any scored rac
es before their sons started running. And now, the dad has completed over 40 races (the majority with one of his sons) and the mom has completed at least a dozen races, often running as fast as she can to keep up with her speedy sons!
Running has become the focal point of many Eden II families. In addition to the running club in school, many families have connected with volunteer coaches and spend evenings running and weekends competing in neighborhood races. Running has not only resulted in increased fitness, but has opened the doors for inclusion in community activities for both participants and their families.
Linda, how can someone manage the program? How do you know if a fitness routine is working?
Fitness programs are managed through data collection and analysis of data summaries over time. It is important to continue to do what is working and stop doing what is not working. A personal fitness trainer should periodically conduct and summarize formal fitness assessments to determine if the participant is meeting fitness goals.
Systematic problem solving is required when fitness goals are not being met. A personal fitness trainer will review the components of the exercise routine to determine if the individual engages in an exercise activity often enough (frequency), long enough (duration), and at a level and amount (progression-overload) required to improve fitness levels.
Revisions may be necessary after reviewing the initial screening results. A personal fitness trainer can revisit the data to determine if the original goals of the programs were appropriate, specific and attainable.
A medical consultation might be required to discern if the participant has developed any additional health concerns which could negatively impact the potential benefits of the workout. A consultation may include measuring the individual’s improved medical status (e.g., decreased blood pressure, lower resting heart rate).
Just the thought of collecting data can be overwhelming and intimidating for many. Can you explain why data is collected, and suggest some easy-to-use tracking systems?
Don’t be intimidated by the thought of taking data. Data are taken for a variety of reasons and can be collected in a variety of ways. For many purposes, exercise journals (e.g., Monday, September 24th, ran for 1.5 miles in 12 minutes) and workout checklists (noting activity, duration, and intensity) are tools that may be used to assess progress and assist in problem-solving over time. Body measurements, weight, and calculating BMI can help determine if the activity you selected to meet your goals of losing fat and increasing lean body mass is working.
An overarching goal for many of our participants is to increase independence in their workouts. Certainly decreasing support levels should be everyone’s goal. A standard checklist noting levels and types of prompts is useful. It is also helpful for the support person to consistently fade prompts. Track the percentage of steps completed independently using a schedule on an iPad. Robert can self-record the number of sit-ups he has completed, how long he ran on the treadmill, and which weights he used on the circuit during a session at the gym. A teacher can record that Martin pinned his bib number to his shirt before the race this morning.
For teaching independence or use of a locker room, a standard task analysis can be conducted. Data can be collected and summarized as the percentage of steps completed independently.
Social validity is another important consideration. Does the participant with autism look like everyone else in the gym or in the community? It is important to keep in mind that typical people may exhibit strange, but acceptable behaviors in the gym and in the community. Are you meeting the goals that the participant and/or those who support the participant have previously agreed are important? A simple social validity assessment could look like this:
Jeff, fitness encompasses many factors that are indeed quite measurable. Can you provide some details about data collection both with respect to independent and dependent variables?
It is common to see personal fitness trainers and participants using timers, counters, clipboards, smart phones or iPads to track their workouts in the gym and on the track. They record: the type of strength training exercise; the weight lifted; the number of repetitions and sets in the gym; the number of laps or total distance on the road and in the pool. It is also important to record machine settings (e.g., treadmill speed and incline, seat positions on exercise equipment) to enable safe and consistent exercising.
Record all workout sessions as they occur (e.g., date, type). Data should be collected at least 1x per week on each individual skill. If the individual does three sets during a strength training session, you may choose to collect data on only the first set. If the individual uses a variety (e.g., intervals, distance), of aerobic workouts in their schedule, record each in a journal.
Fitness change is gradual, but prompting levels might vary. Record the last prompt level/location used so you know where to start on the first repetition of the next session.
Jeff, at the start of the interview, we talked a bit about future research addressing the suppression of stereotypy and other behaviors. Can you share with our readers your broader ideas about future research related to fitness in general?
There are a number of areas warranting further research:
- With respect to strength training: scientifically validated protocols to teach proper use of exercise equipment and then to increase independent use of the equipment would be very beneficial.
- The gym or many exercise settings (studios, trails, tracks, and pools) are novel (not part of the person’s learning history) and can be a place to teach skills that were never mastered elsewhere. It will be important to demonstrate both from a research standpoint, as well as clinically, that the skills mastered in the gym or track, generalize to school, home, and community settings.
- Is it possible to increase the number of social interactions in community-based exercise settings through peer modeling or observational learning?
Linda, what do you see as additional areas for future research?
I was invited to participate in a research team’s efforts to replicate and expand upon previous studies regarding the benefits of fitness activities and the impact on stereotypy, aggression and increased attention during academic tasks. Therefore, it would be helpful for future research to assess the extent to which gains extend beyond the acquisition of fitness behavior but also lead to improvement in other desired behaviors.
Thank you both for a wonderfully thorough interview. Your experiences in the field, or shall I say in the gyms and on the field are clearly conveyed and for that I am very grateful. You have shared an incredible amount of information that would be helpful to all. The extensive listing or resources will be of great use to new researchers eager to tackle some many of the unanswered questions related to fitness training for individuals with autism.
ADDITIONAL EXERCISES:
Linda Meyer, Ed.D., MPA, BCBA-D, CPT is a consultant in private practice (Linda S. Meyer Consulting LLC). She is the cofounder of the Alpine Learning Group in Paramus, NJ and served as its founding executive director from 1989 until 2005. She serves on the professional advisory boards of several schools and agencies serving individuals with autism spectrum disorders. Linda has presented at regional, national, and international conferences, and authored articles and book chapters on various special education, nonprofit management, and personal fitness topics. She provides consultation in community-based fitness instruction for adolescents and adults with autism spectrum disorders. She has taught doctoral and Masters level students (in educational and clinical psychology programs), and is currently an adjunct professor at Caldwell College, in Caldwell, NJ. Linda is a member of the NJ Governor’s Council for Research and Medical Treatment of Autism.
Jeff Jacobs, MA, BCBA is a behavior analyst who works in the Hackensack School District in New Jersey. He has been teaching Tae Kwon Do to individuals diagnosed with ASDs for more than 15 years. Jeff provides private consulting and community-based fitness instruction. He has presented at regional and national conferences on fitness, using iPad/iTouch to increase independence, and the use of correct technique during rigorous exercise routines.
References
Ahearn, W.H., Clark, K.M., MacDonald, R.P.F., & Chung, B.I. (2007). Assessing and treating vocal stereotypy in children with autism. Journal of Applied Behavior Analysis, 40, 263–275.
American College of Sports Medicine. (2010). Guidelines for exercise testing and prescription (8th ed.). Philadelphia: Lippincott, Williams, & Wilkins.
Baranek, G. T. (2002). Efficacy of sensory and motor interventions for children with Autism. Journal of Autism and Developmental Disorders, 32, 397-422.
Celiberti, D.A., Bobo, H.E., Kelly, K.S., Harris, S.L., & Handleman, J.S. (1997). The differential and temporal effects of antecedent exercise on the self-stimulatory behavior of a child with autism. Research in Developmental Disabilities, 18, 139-150.
Cooper, J. O., Heron, T. E., & Heward, W. L. (2007). Applied behavior analysis (2nd ed.). NY: MacMillan.
Elliot R.O., Dobbon, A.R., Rose, G.D., & Soper, H.V. (1994). Vigorous aerobic exercise versus general motor training activities: Effects on maladaptive and stereotypic behaviors of adults with both autism and mental retardation. Journal of Autism and Developmental Disorders, 24, 565-576.
Fragala-Pinkham, M., Haley, S. M., & O’Neil, M. E. (2008). Group aquatic aerobic exercise for children with disabilities. Developmental Medicine & Child Neurology, 50, 822–827.
Kern, L., Koegel, R. L., & Dunlap, G. (1984). The influence of vigorous versus mild exercise on autistic stereotyped behaviors. Journal of Autism and Developmental Disorders, 14, 57–67.
Kern, L., Koegel, L. R., Dyer, K., Blew, P. A., & Fenton, L. R. (1982). The effects of physical exercise on self-stimulation and appropriate responding in autistic children. Journal of Autism and Developmental Disorders, 12, 399–419.
Kohrt, W.M., Bloomfield, S.A., Little, K.D., Nelson, M.E., & Yingling, V.R. (2004). Physical activity and bone health. Medicine & Science in Sports and Exercise, 36 (11), 1985-1996.
Lang, R., Koegel, L., Ashbaugh, K., Regester, A., Ence, W., & Smith, W. (2010). Physical exercise and individuals with autism spectrum disorders: A systematic review. Research in Autism Spectrum Disorders, 4, 565–576.
Levinson, L. J., & Reid, G. (1993). The effects of exercise intensity on the stereotypic behaviors of individuals with autism. Adapted Physical Activity Quarterly, 10, 255–268.
Lochbaum, M., & Crews, D. (2003). Viability of cardiorespiratory and muscular strength programs for the adolescent with autism. Complementary Health Practice Review, 8, 225–233.
Meyer, L. S., & Jacobs, J. (2007). Checklist to assist individuals with autism spectrum disorders or caregivers in the selection of fitness, leisure, and recreation programs. The Association for Behavior Analysis International Autism Special Interest Group Newsletter, 23, 8-12.
Nelson, M.C., Gordon-Larsen, P. Adair, L., & Popkin, B. (2005). Adolescent physical activity and sedentary behavior. American Journal of Preventive Medicine, 28, 259-266.
Nicholson, H., Kehle, T.J., Bray, M.A., & van Heest, J. (2011). The effects of antecedent physical activity in
the academic engagement of on children with autism spectrum disorder. Psychology in the Schools, 48, 198-213.
Pan, C.Y. (2010). Effects of water exercise swimming program on aquatic skills and social behaviors in children with autistic spectrum disorders. Autism, 14, 9-28.
Pitetti, K.H., Rendoff, A.D., Grover, T. & Beets, M W. (2007). The efficacy of a 9-month walking program on the exercise capacity and weight reduction for adolescents with severe autism. Journal of Autism and Developmental Disorders, 37, 997-1006.
Powers, S., Thidabeau, S., & Rose, K. (1992). Antecedent exercise and its effect on self-stimulation. Behavioral Residential Treatment, 7, 15-22.
Prupas, A., & Reid, G. (2001). Effects of exercise frequency on stereotypic behaviors of children with developmental disabilities. Education and Training on Mental Retardation and Developmental Disabilities, 36, 196-206.
Rosenthal-Malek, A., & Mitchell, S. (1997). Brief report: The effects of exercise on the self-stimulatory behaviors and positive responding of adolescents with autism. Journal of Autism and Developmental Disorders, 27, 193- 202.
Sowa, M., & Meulenbroek, R. (2012). Effects of physical exercise on autism spectrum disorders: A meta-analysis. Research in Autism Spectrum Disorders, 6, 46-57.
U.S. Department of Health and Human Services. (1999). Physical activity and health: A report of the Surgeon General. Retrieved from http:www.cdc.gov/nccdphp/sgr/prerep.htm.
Watters, R. G., &.Watters, W. E. (1980). Decreasing self-stimulatory behavior with physical exercise in a group of autistic boys. Journal of Autism and Developmental Disorders, 10, 379–387.
Yamaki, K. (2005). Body weight status among adults with intellectual disability in the community. Mental Retardation, 43, 1-10.
Yanardag, M., Birkan, B., Yilmaz, I., Konukman, F., Agbuga, B., & Lieberman, L. (2011). The effects of least to most prompting procedure in teaching basic tennis skills . Kinesiology, 43 (1) 44-55.
Yilmaz, I., Yanardag, M., Birkan, B.A., & Bumin, G. (2004). Effects of swimming training on physical fitness and water orientation in autism. Pediatrics International, 46, 624-626.
Thanks to The Association For Science In Autism Treatment for granting permission to republish this article.
– See more at: http://autismbeacon.com/topics/article/everything_you_wanted_to_know_about_fitness_training_for_adults_with_autism/physical_fitness_general_health_wellbeing#.UbmOQpUm6j4