There hasn’t been a Medicaid rate adjustment for behavioral health providers since 2007, this means screening, diagnosis, and treatment of autism is considered charity care by most providers. Here’s one example of one category of behavioral health care provider:
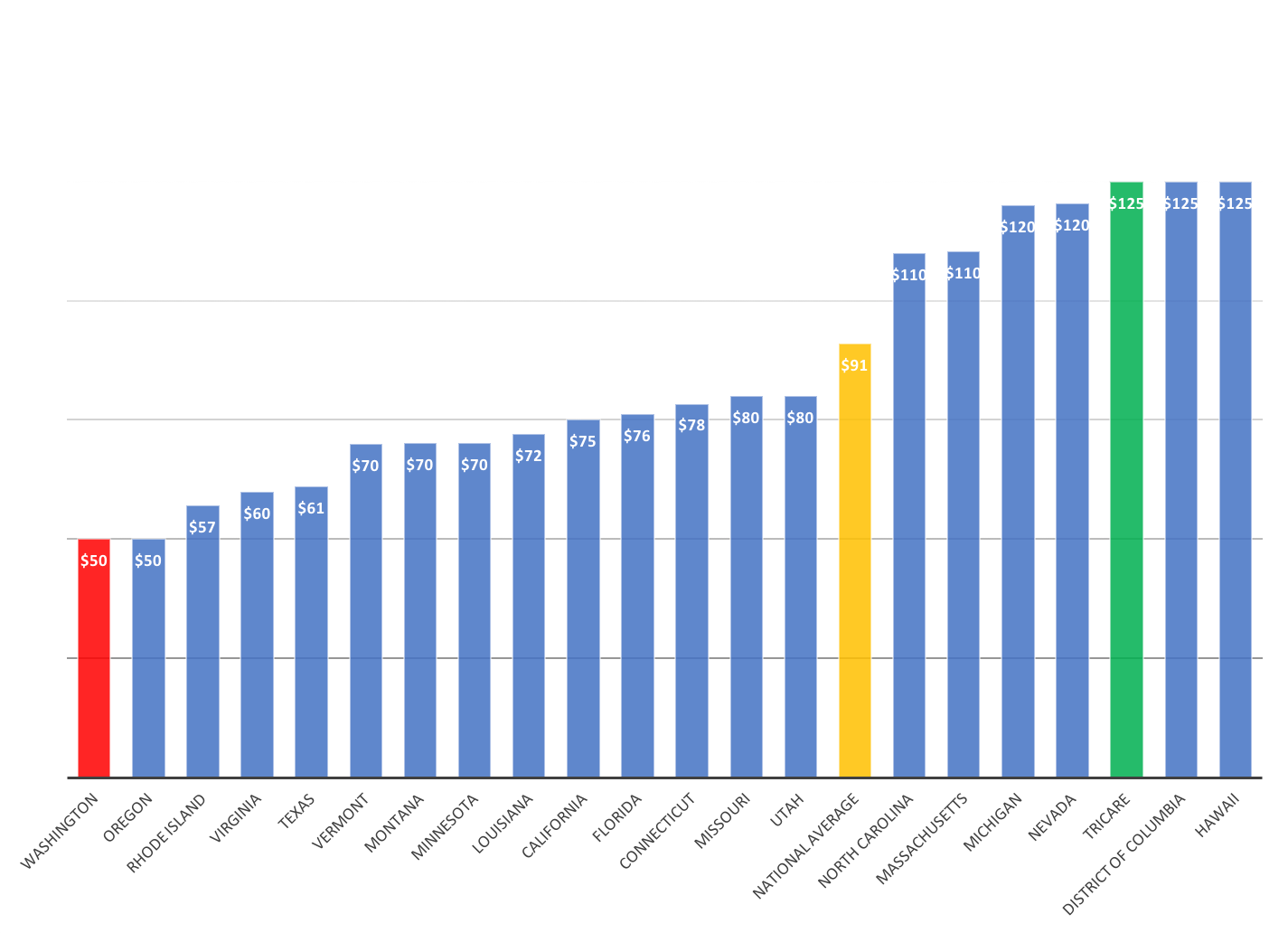
Red is WA Medicaid rate, lowest in the nation, yellow is the national average, and green is Tricare’s rate which is comparable to private health benefits, it’s 2.5 times higher than the WA Medicaid rate. It’s not surprising that private insurance and private health plans have a much more robust network of providers in comparison to Managed Care plans.
SB 5828 – Increases payment for Medicaid home health services to no less than one hundred percent of the medicare rate. Provides for reimbursement for a social worker and telemedicine under the medicaid home health benefit. Creates a work group to redesign the home health reimbursement payment methodology.
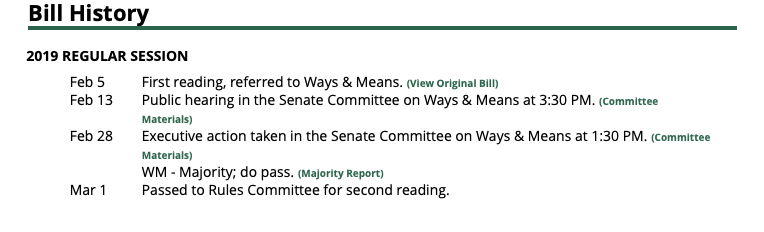
A similar bill in the House HB 1185 – Requires a Medicaid payment for health care services furnished by a licensed health care provider, with either a provider contract with the state health care authority on a fee-for-service basis or under a contract with a Medicaid managed care organization, to be at a rate not less than one hundred percent of the payment rate that applies to those services and providers under Medicare.
Regrettably, HB 1185 has not been given a hearing yet.
If your family has been impacted adversely by Medicaid reimbursement rates, either for behavioral health for home health services, and wish to share your story with legislators, please sign up as a WAAA Ambassador via email [email protected] or by phone at 425-894-7231.
Thank you for Standing together with us for Change!